| Al-Hamed et al. (2017)23
|
PRF showed overall positive results for pain, trismus, edema, periodontal pocket depth, soft tissue healing, and localized osteitis incidence. The meta-analysis could not be performed for all variables. The meta-analyses did not show significant benefits for PRF compared to natural healing sockets. |
Considering the limitations of the available evidence, PRF does not seem beneficial for bone consolidation after lower third molar extractions. Further controlled and standardized randomized clinical trials are required to estimate the effect of PRF on socket regeneration. |
| Bao et al. (2021)27
|
A-PRF showed a better effect among the three groups for the improvement of postoperative pain on the third and seventh days. L-PRF promoted soft tissue healing on the seventh day compared to the control. However, other comparisons did not show significant differences. |
Limited results showed that applying A-PRF after third molar extraction reduced postoperative pain, and L-PRF promoted soft tissue healing on the seventh postoperative day. However, the positive impact on other postoperative sequelae was not confirmed. Further large-scale randomized controlled trials with uniformly standardized measuring methods are required to improve the analyses. |
| Bao et al. (2021)28
|
PRF showed significant positive effects on pain, edema, soft tissue healing, trismus, and alveolar osteitis. There was no statistically significant effect on bone healing. |
Limited clinical evidence indicates that applying PRF after lower third molar extraction may reduce pain, edema, trismus, and dry socket alveolitis and promote soft tissue healing. However, the effect of PRF on bone healing requires further large-scale randomized controlled trials with uniform measuring criteria. |
| Barona-Dorado et al., (2014)15
|
Gürbüzer et al., 2008: No statistically significant differences. Rutkowski et al., 2010: PRP showed significantly smaller facial edema and higher bone density. Haraji et al., 2012: PRP showed significantly lower post operative pain, improved healing, and lower postoperative alveolar osteitis incidence. |
The scientific evidence for using PRP in third-molar surgeries is scarce. Hence, randomized clinical trials are required before recommending the clinical application of PRP. |
| Canellas et al. (2017)16
|
PRF seemed to accelerate healing in mandibular third molar surgeries, reducing postoperative pain and edema. PRF significantly decreased alveolar osteitis prevalence. |
Although further well-designed clinical trials with larger samples are required to allow definitive conclusions, PRF is a potentially suitable biomaterial. |
| Canellas et al. (2019)25
|
PRF showed significantly better bone regeneration for alveolar cleft reconstruction, decreased alveolar osteitis prevalence, and increased implant stability one week and one month after surgery. |
PRF may present improved wound healing when used in oral surgical procedures. The most consistent indications of this systematic review are to preserve alveolar dimensions after extraction and to reduce alveolitis incidence after lower third molar surgery. |
| Costa et al. (2023)32
|
A-PRF and L-PRF resulted in lower pain levels on the first and third postoperative days compared to the blood clot. On the seventh postoperative day, pain was significantly lower for A-PRF, L-PRF, and PRP compared to the blood clot. There was a statistically smaller difference in the reduction of interincisal opening for A-PRF compared to L-PRF and the blood clot during the acute inflammatory period. A-PRF, L-PRF, PRP, and CGF demonstrated favorable outcomes in reducing edema in at least one evaluated period. |
Given the low quality of evidence, A-PRF following lower third molar extractions demonstrated superior performance among the analyzed blood concentrates and appeared effective in reducing postoperative pain at all evaluated time points. Trismus decreased with the use of A-PRF during the peak inflammatory period. |
| Fujioka-Kobayashi et al. (2021)17
|
PRF significantly reduced the alveolar osteitis rate from 15.9% in the control group to 5.8% in the PRF group, representing an approximated three-fold reduction. PRF showed better results for soft tissue healing. |
PRF decreases postoperative pain/morbidity, favors soft tissue healing, and presents lower complication rates of alveolar osteitis. Therefore, PRF represents a feasible auxiliary treatment after lower third molar removal. |
| He et al. (2017)27
|
PRF significantly relieved pain, reduced edema on the third postoperative day, and decreased alveolar osteitis incidence. There were no significant differences in swelling on the first postoperative and bone consolidation day. |
The local application of PRF after lower third molar extraction is a valid method to relieve pain and edema at three postoperative days and reduce alveolar osteitis incidence. For patients subjected to complicated surgical extractions, PRF may be recommended for local socket applications. |
| Ramos et al. (2022)30
|
L-PRF showed better pocket depth, insertion level, and pain control (first and third days), but it was not associated with improved soft tissue healing on the seventh day. A-PRF presented lower analgesics intake. L-PRF and A-PRF controlled edema better but not trismus. |
Using L-PRF and A-PRF allows better pain and edema c ontrol than standard PRF protocols, but none affected trismus. PRF and L-PRF protocols improved soft tissue healing but not to a statistically significant degree. However, they improved probe depth in the third month after the third molar surgery. |
| Ribeiro et al. (2024)36
|
Using L-PRF contributed to reduce postoperative pain and discomfort. |
The L-PRF considerably reduced postoperative pain, edema, alveolar osteitis incidence, and infections following third molar removal surgery compared to patients not subjected to L-PRF application. |
| Snopek et al. (2022)31
|
PRF favored the reduction of alveolar osteitis frequency and had an uncertain effect on the level of postoperative pain, edema, and wound healing. Pain levels did not show statistical differences. |
Considering the low number of included studies, the effect of PRF after lower third molar surgery could not be evaluated. Further studies should focus on a higher methodological quality to produce reliable and comparable study results. |
| Vitenson et al. (2022)18
|
A-PRF caused significantly lower pain scores than L-PRF and natural wound healing after two, three, and seven days. A-PRF had a significant effect on facial edema and trismus and some positive effects on soft tissue healing. |
The included studies were characterized by considerable heterogeneity and confounding variables. Thus, the level of evidence seems inadequate for clinical recommendations according to the focus question. |
| Xiang et al. (2019)26
|
PRF relieved pain and edema and reduced alveolar osteitis incidence. There was no statistical difference for trismus and bone and soft tissue healing. |
PRF reduces only some postoperative complications, but it does not prevent all of them. PRF significantly relieved pain and edema and reduced alveolar osteitis incidence after extracting an impacted lower third molar. |
| Zhu et al. (2021)29
|
PRF significantly reduced alveolar osteitis incidence and postoperative pain (first, third, and seventh days) compared to the controls. |
Besides reducing alveolar osteitis incidence and postoperative pain after third molar surgery, it may also improve postoperative healing of soft tissues. |

 Performance of blood concentrates in controlling inflammatory signs and symptoms after lower third molar extractions: an overview
Performance of blood concentrates in controlling inflammatory signs and symptoms after lower third molar extractions: an overview Thumbnail
Thumbnail
 Thumbnail
Thumbnail
 Thumbnail
Thumbnail
 Source: Elaborated by the authors.
Source: Elaborated by the authors.
 Source: Elaborated by the authors.
Source: Elaborated by the authors.
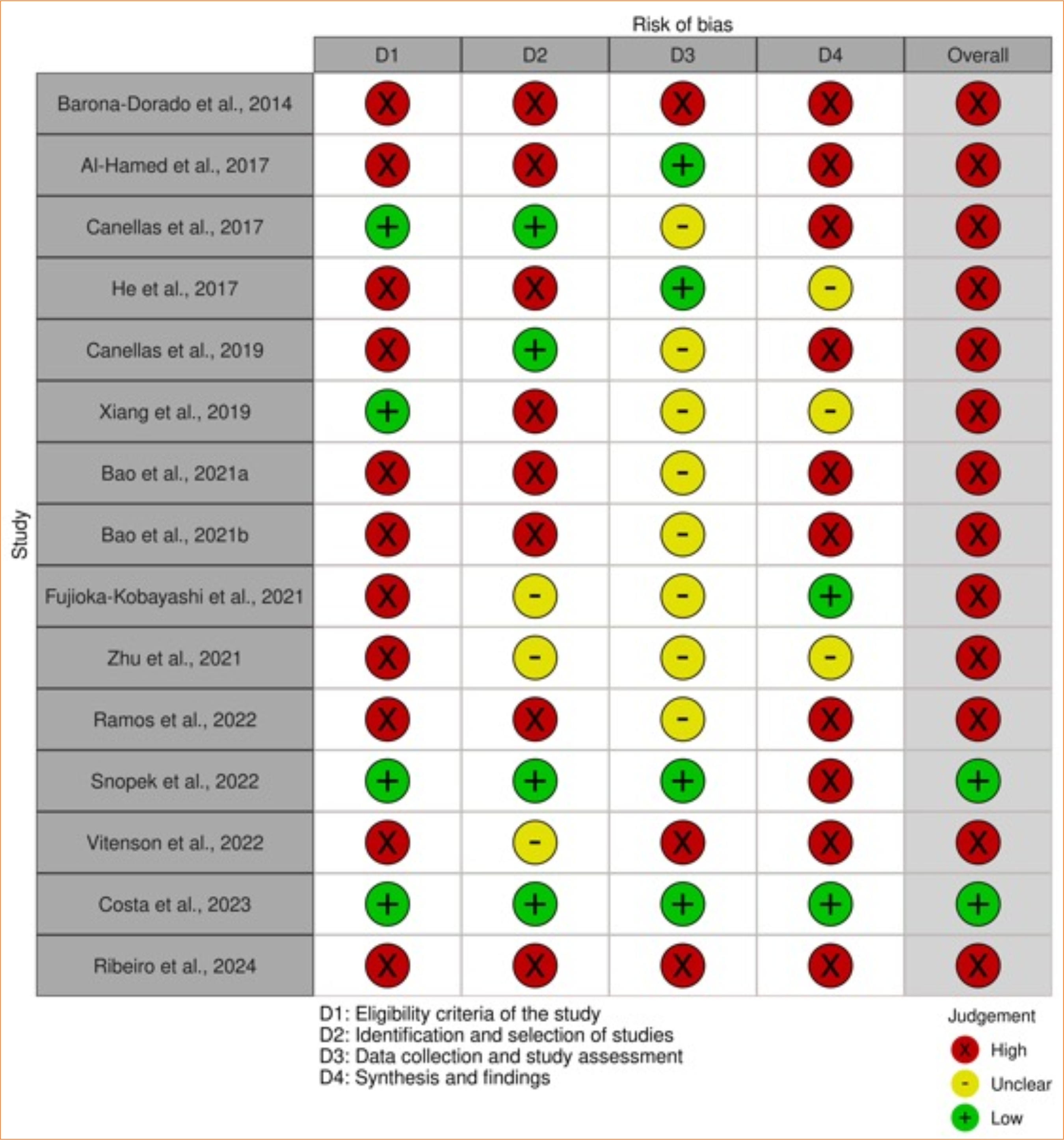 Source: Elaborated by the authors.
Source: Elaborated by the authors.